Let’s face it: Pregnancy can be tough. Between bouts of morning sickness, an aching back, and heartburn that just won’t seem to go away, you need all the TLC you can get during the next few months as a mom-to-be.
Enter a pregnancy survival kit — the lifesaver every pregnant woman needs to get through the next three trimesters until their new baby arrives. A pregnancy survival kit can be a game-changer for an expecting mom in the event of unexpected (or unpleasant) situations during pregnancy. It will help you deal with all the little aches and pains that make pregnancy symptoms such a struggle.
Does this sound familiar to you?
“I always felt like during my pregnancy, I never knew what I might need when I was out and about. I’d pack a small bag of pregnancy necessities and keep it in my car so I always had it with me. I’d throw in easy snacks, an extra set of undies in case I was leaking, some crackers and a Gatorade.”
– Debra K., mama of three.
Whether you spent your last pregnancy wishing you had some extra tools or are a first-time mom and want to be prepared for your first baby, here’s everything you need to know about creating a pregnancy survival kit.
The Essential Items for Any Pregnant Mom
The first things to put in your pregnancy survival kit are essential items such as first aid supplies. A basic first aid kit should include items like bandages, gauze, antiseptic wipes, prenatal vitamin supplements, and pain relievers. If you’re making a pregnancy to-go bag or smaller kit, simplify that to a few baby wipes, bandages, and pregnancy-safe painkillers once you’ve gotten the “all clear” from your doc.
Other essential items include snacks and water — staying hydrated is important. Bring a water bottle or a sports drink with electrolytes wherever you go.
Or maybe you’ll throw a ginger ale, sea bands, or saltine crackers to ease that nausea, especially in the first trimester. To combat that heartburn we all know and don’t love, you have a few possible solutions. Some moms swear by sugar-free gum, yogurt, and doctor-approved meds.
Healthy snacks like fruits, nuts, and granola bars can help ease the cravings and nausea that inevitably come along with being preggo. Hydration, food, and sleep: Those three pregnancy must-haves will go a long toward making the next few months as easy as possible.
Personal Care Items
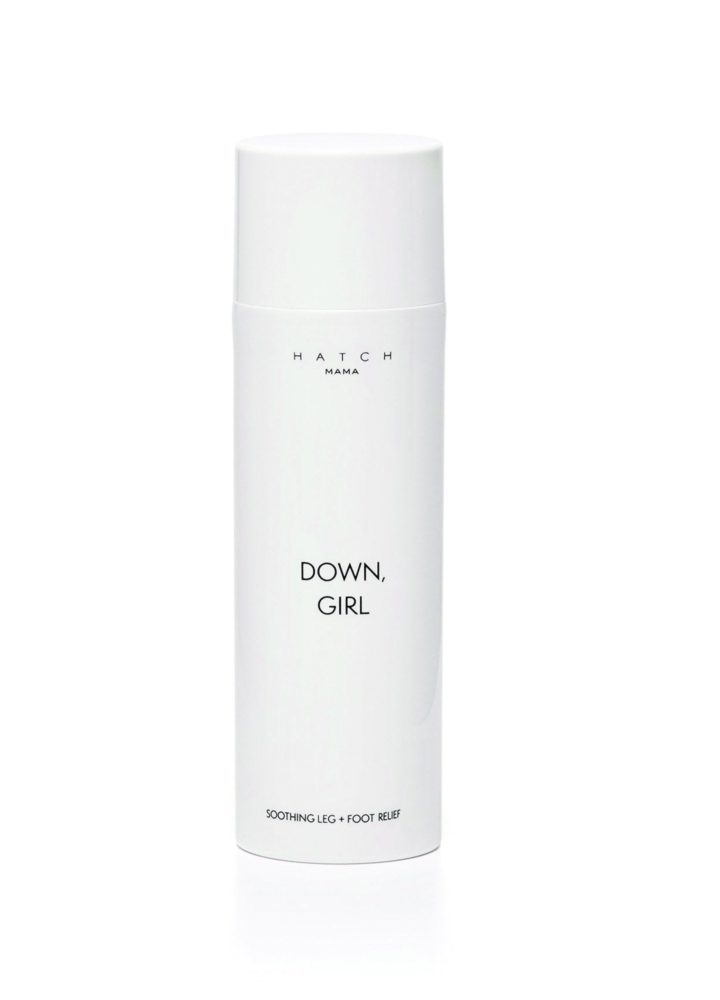
Other items to stash in your new mom survival kit include any personal hygiene items you need to navigate time away from home, such as pads and tissues, rescue balm for your lips and chafing nips, or cooling cream for your swollen feet and ankles.
Add in hair ties, lotion, and a pair of UV-protective sunnies. Don’t forget the hand sanitizer — no need to be picking up germs right now.
You might want to carry around items geared toward self-care. It’s no secret that pregnancy can be rough. Between your mood swings and other pregnancy symptoms, you deserve some pampering.
Aromatherapy tools like essential oils, a beautiful journal to write in, or even a fab set of headphones can make a world of difference when dealing with a difficult pregnancy, especially as the third trimester comes to a close.
Make your life a bit easier by ordering a care package sent straight to your house, like our favorite Mama Must-Haves Kit stocked with best-selling pregnancy essentials. Self-care isn’t an indulgence right now; it’s a priority.
What Type of Hospital Bag Should I Use?
Keep your pregnancy essentials kit in a bag you can easily grab and go, such as a tote or backpack. Choose a bag that you’re going to WANT to grab on the daily. There’s no point in picking an old hiking pack that you hate or a flimsy grocery tote bag you’re not going to carry around with you.
If you love shopping for maternity clothes and accessories (who doesn’t?), this would be a wonderful opportunity to splurge on an oversized purse or bag that you’ve really been wanting. Use it to build your pregnancy survival kit (especially if it matches your baby shower dress).
You might put this bag on your baby registry and receive it as a baby shower gift. This bag is going to be your new best friend for the next nine months (and longer if it can be a diaper bag). We might as well make it something that we enjoy using and wearing!
Speaking of your pregnancy gift registry, remember that you can always build out your pregnancy emergency kit by putting some items on your baby registry, too. You might be busy buying items specifically for your little one, but your baby shower (and baby registry) are also meant for you, too!
Don’t be afraid to include some self-care gift ideas or pregnancy essentials on that list that are just for yourself. A girl needs to relax and take a break from the hard work of pregnancy.
Survival Kit Maintenance
It’s important that you don’t just create your pregnancy survival kit but also that you regularly check and update your essential items, even during the postpartum period. Need a new heating pad? Run out of tissues or tums?
Set a reminder in your phone to restock those as soon as you get home. Mommy brain is a real thing, and you might not be able to count on your memory the way you’re used to, at least for the moment.
It can also help to remember exactly what you need or want to include in your kit if you keep a running list going in your Notes app or on a notepad around your house. That way, every time you think of something you need, you don’t have to rely on yourself to remember it — you can simply add it to the list.
Survive vs. Thrive: Designer Attire for Moms-To-Be
Here’s the bottom line: A pregnancy emergency kit isn’t just an essential item for any expectant mother; it’ll provide the peace of mind you crave right now. Pregnancy is stressful, and packing those essential items and self-care is doing your future self a huge favor.
Sources: